A rather novel two-staged approach to nipple-sparing mastectomy appears to reduce the risk for the most serious potential complications and may expand the procedure to patients who would have been high-risk candidates for NSM, according to new research.
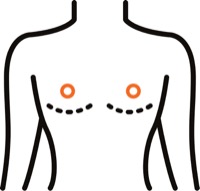
Although there is some controversy about how delayed procedures work, there is little question that they do; for more than 400 years, surgeons have created surgical wounds meant to stimulate the body to enhance blood flow to the wounded area. First described in breast surgery nearly 10 years ago, devascularization of the nipple-areolar complex (NAC) involves dividing the central portion of the breast skin envelope containing the NAC from the underlying breast tissue along the subcutaneous plane, and this is usually performed several weeks before NSM (Ann Surg Oncol 2012;19[10]:3171-3176).
“This allows for compensatory increase in tissue blood flow prior to definitive NSM,” said Tammy Ju, MD, a breast surgical oncology fellow at Stanford University School of Medicine, in California.
Under lead surgeon Irene Wapnir, MD, a breast surgical oncologist and professor of surgery at Stanford, breast surgeons at that institution perform the devascularization procedure by making radial or inframammary fold incisions through which the NAC and central breast skin envelope are separated from the underlying breast tissue.
“The dissection is extended anywhere from 3 cm to 5 cm beyond the areolar edge. Essentially, you just detach the skin; it’s just like making the plane of a mastectomy flap,” Dr. Ju said.
To evaluate the impact of devascularization of the NAC on ischemic outcomes—the most dreaded of which are skin-flap necrosis and nipple loss—Dr. Ju and her colleagues retrospectively reviewed data on patients who underwent either single- or two-stage operations at Stanford between 2015 and 2019.
The single-stage cohort consisted of 67 patients and 103 breasts; the two-stage group consisted of 60 patients and 109 breasts. The mean time between devascularization and NSM in the two-stage group was 32 days, with 12 patients (17.4%) delaying NSM by 84 to 415 days for chemotherapy and locoregional radiotherapy, or due to indecision about their surgery. The same surgical oncologist performed the NSMs, and four plastic surgeons did the post-NSM reconstructions.
Among the 103 breasts in the single-stage cohort, eight (7.8%) had nipple necrosis requiring operative excision; this did not happen to any breasts in the two-stage cohort. In contrast, partial- and full-skin thickness ischemic complications involving the part of the NAC or localized area of the mastectomy flap were similar between the two groups.
Timing appeared to have some impact on the two-stage operation’s success in preventing ischemic complications. Five patients (nine breasts) underwent NSM less than 20 days after devascularization; 55.6% of these breasts developed partial-thickness NAC ischemic complications, compared with 11% in patients who delayed NSM 20 or more days.
“Similarly, mastectomy flap ischemic events were higher for the short-interval group compared with the greater than 20-day group,” Dr. Ju said.
There is a paucity of literature on two-stage NSM and no code for it, but the results of this study have prompted Dr. Ju and her colleagues to offer two-stage NSM to a broader range of patients, such as those with more ptotic and larger breasts, and to advocate that they wait at least three weeks between operations.
“We initially offered two-stage NSM to patients we thought were at higher risk for ischemic complications due to established risk factors. Even knowing those risks, patients who did not want to undergo two surgeries often preferred the single-stage approach; but now, based on our experience, they’re more comfortable waiting a few weeks between surgeries if it can decrease their risk of losing a nipple,” Dr. Ju said.
Going forward, Dr. Ju and her colleagues intend to evaluate long-term outcomes and complications in the surgical delay group to further define ideal candidates for the procedure. She presented the research as a poster at the 2021 annual meeting of the American Society of Breast Surgeons.
Katherine Yao, MD, the chief of the Division of Surgical Oncology at NorthShore University HealthSystem, in Evanston, Ill., told General Surgery News that she and her colleagues do not offer two-stage NSM and would have to think about how this technique would improve outcomes or expand eligibility. As it stands, they do a high volume of NSM and rarely see nipple loss in their patients.
In the technique Dr. Ju described, “they mainly use a vertical and radial-lateral incision, whereas we exclusively use inframammary incisions. I think any incision that stays away from the nipple—that is, inframammary versus vertical and radial—will have a better chance of avoiding nipple loss,” she said.
Potential downsides to the two-staged approach include tumor subtypes where a delay before starting adjuvant therapy would be unwanted, and OR issues. “Scheduling two separate procedures is a real issue for us, and I imagine it would be for many surgeons,” Dr. Yao said.
“So, I’m not sure we would adopt this technique at our institution. However, this technique may play a role for some patients. Success of NSM is really about patient selection.”
This article is from the August 2021 print issue.



Please log in to post a comment