Many patients experience pain postoperatively related to their surgery. Unfortunately, far too many operations result in a surgical site infection. Doctors and hospitals may say infections following surgeries are a potential risk, but for many, postsurgical infections can be the result of contaminated treating environments and/or negligence. In the United States, approximately 27 million surgical procedures are performed each year, with as many as 5% of those resulting in an SSI.1
Contamination within an OR can be introduced through a variety of sources: surgical instruments and equipment, personnel and the patient, inanimate objects and surfaces, the air and even insects, potentially causing harm. To provide a safe environment for both the patient and health care worker, an environmental control program should be established for the OR to keep microorganisms to a minimum.
In 2017, the American College of Surgeons and Surgical Infection Society published SSI guidelines found that they are the most common and costly type of health care–associated infection (HAI) and accounted for 20% of all HAIs. The annual incidence of SSI in the United States is between 160,000 and 300,000, or 2% to 5% of patients undergoing inpatient surgery, and the attributable health care cost ranges from $3.5 billion to $10 billion annually. On average, an SSI increases a hospital length of stay by 9.7 days.2
The recommendations put forth by the Association for peri-Operative Registered Nurses, and the Association for the Healthcare Environment’s Practice Guidance for Healthcare Environmental Cleaning, are the standards used by most health care facilities in setting up their infection prevention procedures regarding the OR and other procedural spaces. However, as a consultant, I have provided hundreds of OR assessments across the country, and have often found cleanliness and infection prevention practices to be lacking. Preoperative leaders are not maintaining their ORs to industry standards, and after interviewing surgeons they had no clue of the problems.
Cleaning measures are needed before, during and after surgical procedures (in between procedures), and at the end of each day. Such cleaning must be considered an environmental essential, and infection prevention considerations should include the following:
Air handling or ventilation systems of the surgical suite should be designed to minimize contaminants. Air entering the room through the HVAC system should originate from the ceiling and exit through the return near or at the floor. Air exchanges should be a minimum of 15 per hour with at least four of those air exchanges originating from a fresh air source, and be HEPA filtered. Many hospitals have increased their air exchange rates to as high as 25 per hour with 100% of those being fresh air.
Proper attire (scrubs) should be freshly laundered and donned at the hospital to reduce the number of contaminants carried in from outside of the OR. Because scrubs are considered a form of personal protective equipment, they should be taken off prior to health care workers leaving for the day.
Traffic during the operation should be confined to the members assigned to that procedure. The microbial levels in the air are directly proportional to the number of people moving about and talking within the OR. Minimizing the number of people in the room, or how many times members of the team enter or exit throughout the procedure can help reduce infection rates.
Bloodborne pathogens have the potential to be infectious, as well as other body fluids including saliva; cerebrospinal, synovial, pleural, pericardial, peritoneal and amniotic fluids; semen; and vaginal secretions. Caution should be taken when handling specimens, organs (other than intact skin), and cell or tissue cultures.
Employing New Technologies
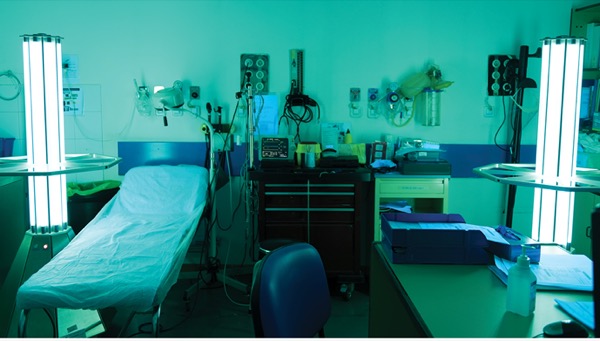
New technologies are designed to help keep ORs cleaner and can include products with ultraviolet light and advances in heating, ventilation and HVAC systems, such as needlepoint bipolar air ionization (NPBI) technology. What are the pros and cons of using these technologies?
According to the Environmental Protection Agency, indoor air can be two to five times more polluted than outside air.3 A newer technology, NPBI produces a high concentration of positive and negative ions, which allows similarly charged particles to combine (get larger), making it easier for them to be filtered more effectively. Basically, as the ions travel within the airstream, they attach to pathogens, particles and gas molecules, breaking them down and rendering them ineffective.
Ultraviolet light technology has been thoroughly vetted and has a proven track record since the 1940s. The technology works by using UV-C band wavelength to degrade organic material and inactivating microorganisms and pathogens. Use of the UV-C band energy to inactivate microorganisms is often referred to as UV germicidal irradiation. Many companies are now offering this technology for use in hospitals and other industries. In the wake of the COVID-19 pandemic, UV technology has been used more extensively, but unfortunately there are limitations for its use. Because UV radiation exposure is hazardous to humans, it is typically used in one of four configurations: in unoccupied room disinfection, upper room disinfection, air handler unit surface disinfection and air handler surface airstream disinfection.4
Whether or not an infection rises to the level of medical malpractice will depend on the circumstances surrounding how and when the infection occurred. Medical malpractice cases can be difficult to prove; nevertheless, surgeons should be aware of preventive measures and call on their hospital leadership to do everything in their power to ensure patients remain safe and free of infection.
References
- Hospital infection control: surgical site infections. http://bit.ly/3qYmYbX
- Ban KA, Minei JP, Laronga C, et al. American College of Surgeons/Surgical Infection Society surgical site infection guidelines–2016 update. Surg Infect (Larchmt). 2017;18(4):379-382.
- Indoor air quality: what are the trends in indoor air quality and their effects on human health? http://bit.ly/2O1UNKX
- UVGI vs. BPI: which air-cleaning technology is best for your building? http://bit.ly/3bHUfBZ
David L. Taylor III, MSN, RN, CNOR, is the principal of Resolute Advisory Group, LLC, a health care consulting firm in San Antonio. He can be reached at DavidTaylor@ResoluteAdvisoryGroup.com.
This article is from the March 2021 print issue.


Please log in to post a comment