By Caroline Helwick
Although trigeminal neuralgia (TN) is most common in people over 50 years of age, children represent about 1.5% of the affected patient population. Current treatment options can sometimes have lackluster results, but a recent series of pediatric patients undergoing microvascular decompression (MVD) determined that outcomes could be better than previously thought.
“MVD surgery can be almost as effective for pediatric TN as for adults, if one acts early and aggressively addresses all of the more complex vascular anatomy encountered,” said Mark E. Linskey, MD, a professor of neurological surgery at the University of California, Irvine.
“Trigeminal neuralgia is rare in children, but it does exist,” he noted. The youngest reported case treated surgically was 13 months old, he said. A Facebook support group, called “Families Understanding Trigeminal Neuralgia,” currently has 108 registered children from seven countries.
Anticonvulsants, tricyclic antidepressants and outpatient procedures like radiofrequency ablation, among others, are all usual treatment options for TN. Although more invasive than the other therapies, studies in adult patients have found better results with MVD, according to the National Institutes of Health. In the procedure, a surgeon moves the blood vessel pressing on the nerve and places a cushion between the two, resulting in pain relief.
At the 2019 Conference of the Facial Pain Association, Dr. Linskey described the challenge in diagnosing and treating children with TN. He also reported preliminary results from his series of young patients undergoing MVD.
Based on encouraging findings, he said, “The paradigm that surgical intervention in the form of MVD should only be considered after failure of medical therapy has to be rethought for pediatric TN. At a young age, the syndrome has higher costs to the patient and the medications have far more damaging consequences,” he said.
Few Reports in the Literature
“There are only three published reports in the peer-reviewed literature regarding pediatric trigeminal neuralgia. Quite frankly, the results are discouraging,” Dr. Linskey said.
In the first study, reported by neurosurgeons who originated MVD surgery in adults, 22 patients developed TN as children but received surgery at a median age of 29 years (Neurosurgery 1998;43[4]:804-807). The results were initially encouraging, with “excellent” outcomes in 73% of patients, but declined to 43% after 8.8 years of follow-up.
In the second study, involving seven patients from Oregon Health Sciences Center, in Portland, who were diagnosed before age 25 years, only 50% were pain-free initially and only 14% had excellent results at one year (J Neurosurg 2011;114[5]:1306-1311).
The third study was led by former pediatric neurosurgeon and current secretary of the Department of Housing and Urban Development, Ben Carson, MD, who hypothesized that the worse outcomes could be due to the long duration of symptoms and that intervention in childhood would be more effective. In his study of five patients who underwent MVD at an average age of 12 years, 83% had excellent outcomes but the median follow-up was only one year (Childs Nerv Syst 2011;27[12]:2123-2129). “We had no idea if these promising results were durable or not,” Dr. Linskey said.
Encouraging Results in UC Irvine Series
More promising results have been achieved in Dr. Linskey’s own series, which now includes 50 patients treated since 2006 in his practice, with surgery performed before age 21. Of these patients, 53% had classical TN (100% typical symptoms, characterized by extreme, sporadic pain); 29% had TN type 1 (>50% typical, <50% atypical symptoms, usually distinguished by lower-intensity pain that is constant); and 18% had TN type 2 (>50% atypical, <50% typical symptoms). Patients’ median age at onset was 15 years (range, 13 months to 16 years) and median symptom duration was 22 months (range, five months to seven years).
In a subset of 32 patients having 50 MVDs, neurosurgery in all cases revealed an offending lesion. More than 97% had compression by multiple vessels; 97% had venous compression; and 34% had no named arterial compression (three patients had veins alone and nine had veins plus unnamed artery branches).
Early pain outcomes in 39 patients (first MVD, 25; reoperation, 14) found all patients to be initially pain-free after MVD, with a Barrow Neurological Institute (BNI) Pain Intensity Score of 1 (no pain, no medication); as of last follow-up, this remained at 59% after the first MVD and 29% after a second MVD. BNI class 1 or 2 (occasional pain, no medication) was reported at last follow-up by 72% and 50%, respectively, and BNI 1, 2 or 3 (some pain, adequately controlled with medication) was achieved by 91% and 93%, respectively. Only three patients (9%) had pain not adequately controlled with medication. “Less than 10% of our patients were left with an unacceptable level of improvement,” Dr. Linskey commented.
Lessons Learned About TN in Children
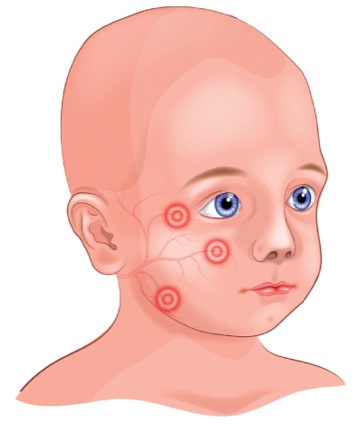
Childhood-onset TN differs in some ways from adult-onset TN. Bilaterality is observed in about 50% of pediatric patients versus 5% of adults. Other cranial nerve syndromes also are more common, especially in patients with bilateral disease. These syndromes were found in 51% of Dr. Linskey’s patients, including geniculate neuralgia (episodic ear pain) and intractable singultus. More than 34% of patients also had other conditions that may or may not be related to TN, such as severe autism and Asperger syndrome, Ehlers-Danlos syndrome, congenital cataracts and glaucoma, pseudotumor cerebri, and other rare disorders.
The vascular anatomy is complex, often involving multiple vessels, large vein contributions and unusual vascular findings, Dr. Linsky said. “There was only one case where a single blood vessel—the superior cerebellar artery—was etiologic. … The majority of patients had multiple vessels and they were not all visible on MRI. All but one patient had venous compression, and multiple veins were very common,” he said. “This is a different entity than TN in adults. Clearly, there are other things that can be contributing biologically to this problem.”