By Ted Bosworth
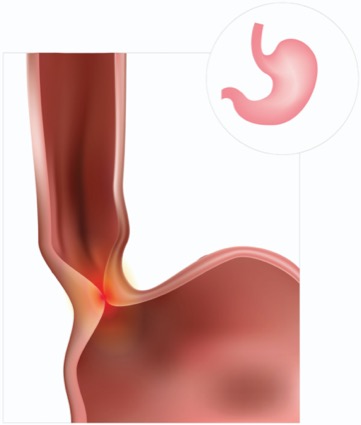
The laparoscopic Heller-Dor procedure provided indefinite control of esophageal achalasia in a majority of patients, according to a series with a median follow-up of 20 years. For some patients, the procedure appears to be a cure.
Largely based on immediate relief of symptoms and relatively short-term follow-up, the laparoscopic Heller-Dor procedure is widely considered a gold standard for surgical control of achalasia, according to Mario Costantini, MD, of the University of Padua School of Medicine, in Italy. However, long-term data have been lacking.
“Little is known of the natural history of the operative patients in the long run, which was the objective of this study,” Costantini said. The new data—a collection of outcomes on all patients treated at his center over a seven-year period in the late 1990s—were submitted to the 2020 Digestive Disease Week (abstract 297).
Of the 87 patients for whom there was a minimum follow-up of 10 years, symptoms recurred one or more times in only 23 (26.4%), Costantini reported. The earliest recurrence was a month after the procedure. One patient with multiple recurrences was still experiencing symptoms 13.5 years after the procedure.
Sixty-four patients remained asymptomatic throughout follow-up. Seven of these patients had died 11 to 24 years into the follow-up period, but none of the deaths among those without recurrent symptoms was considered related to the underlying cause of achalasia. In a patient who died of the underlying cause of achalasia, which was esophageal squamous cell carcinoma, symptoms recurred within one year.
In the remaining 22 patients with recurrent symptoms, three required revision myotomy, but most had adequate control with pneumatic dilations for dysphagia. In one case, a single dilation was offered 10 years after the procedure. In other cases, up to six dilations were administered over the course of follow-up, but these were generally effective, according to the researchers.
“Reflux developed postoperatively, whether endoscopy proven or by pH testing, in only 10 patients,” Costantini reported.
Follow-up endoscopy was recommended every two years. Although not all patients were evaluated this frequently, periodic follow-up was accompanied by a detailed symptom questionnaire that could be scored. Treatment failure was predefined by two criteria: a symptom score greater than the 10th percentile of the preoperative score or the need for further treatment.
The majority of patients were well controlled, regardless of the criteria for success, according to Costantini. He said 92% overall reported satisfaction with the intervention.
Based on these outcomes, the laparoscopic Heller-Dor procedure “represents the reference point with which to match all other treatments,” Costantini said. Although a substantial minority have recurrent dysphagia or other symptoms, control usually is easy to restore.
Although long-term data are always welcome, Peter N. Nau, MD, an associate professor of surgery at the University of Iowa Hospitals & Clinics, in Iowa City, said the Heller-Dor approach may no longer be the gold standard it once was for all comers.
“I do feel strongly that the Heller with fundoplication has an important place in the toolbox of surgeons managing achalasia,” Nau said. In a review of more than 200 cases he included in a review article about laparoscopic Heller myotomy with and without fundoplication (J Xiangya Med 2019;4:12), he found that outcomes were excellent. Still, he said, other approaches should be considered.
“More recently, we have started utilizing POEM [peroral endoscopic myotomy] more often. For an elderly and infirm population and those with type III achalasia, I think this is a potentially better option,” Nau said. “It is less invasive from a cardiopulmonary standpoint and often has a faster return to normal activities.”
In a recent case, he selected POEM for a construction worker who was concerned about lost income during the recovery period.
“The ability to have no lifting restrictions and get back to full work responsibilities for this patient far outweighed the long-term risk of GERD,” Nau explained. However, he added, the choice of procedure has to be individualized. “In a young otherwise healthy patient, I am all for the Heller with fundoplications, because I think it is the best option for both swallowing and reflux control,” he said.


Please log in to post a comment